당화알부민(glycoalbumin) 검사 급여기준
보건복지부 고시 제2020 – 120호
Ⅰ. 행위 제2장 검사료 중 누383 엘라스타제[정밀면역검사]란 다음에 누309 당화알부민[화학반응-장비측정]을 다음과 같이 신설한다.
이 고시는 2020년 7월 1일부터 시행한다.
* 연 2회 급여 인정 – 산정기간 7월 1일 부터 다음해 6월 30일까지 연 2회 (주의!!!)
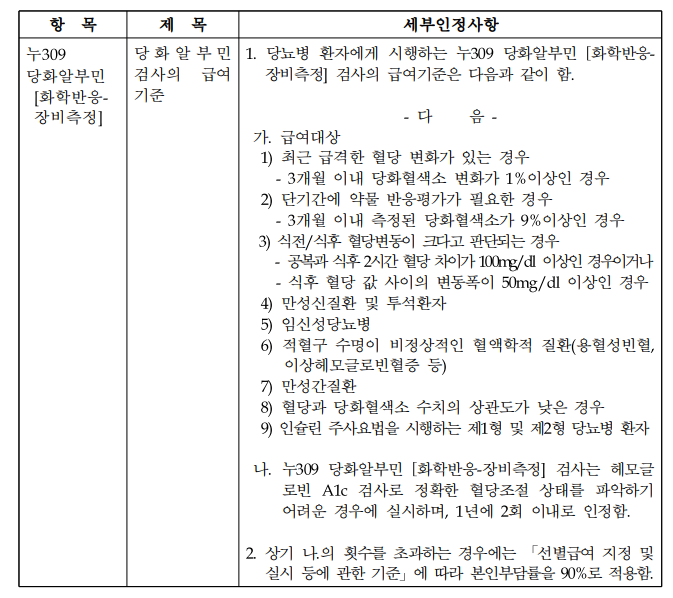
만성 신질환이나 투석환자의 경우 급여 가능
HbA1c 검사로 정확한 혈당조절 상태를 파악하기 어려운 경우에 실시 …
: HbA1c 검사와 같이 시행했을 경우 삭감될 가능성…