COPD Definition
Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.
Diagnosis and Initial Assessment
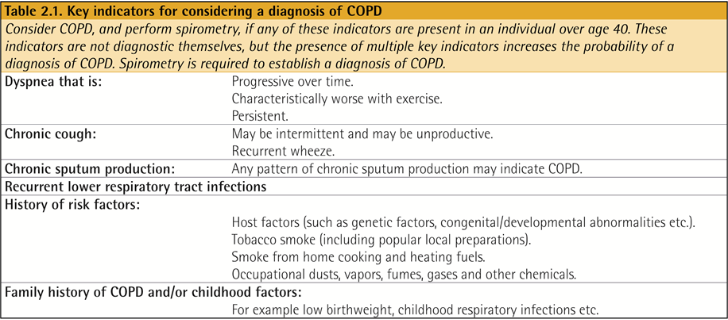
COPD should be considered in any patient who has dyspnea, chronic cough or sputum production, and/or a history of exposure to risk factors for the disease.
Spirometry is required to make the diagnosis; the presence of a post-bronchodilator FEV1/FVC < 0.70 confirms the presence of persistent airflow limitation.
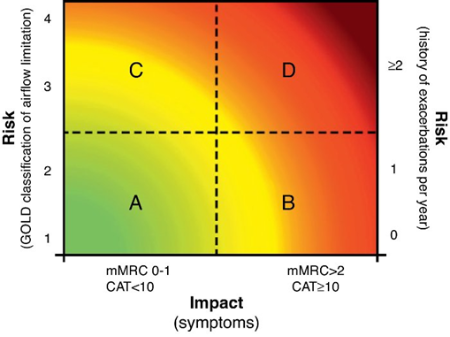
The goals of COPD assessment are to determine the level of airflow limitation, the impact of disease on the patient’s health status, and the risk of future events (such as exacerbations, hospital admissions, or death), in order to guide therapy.
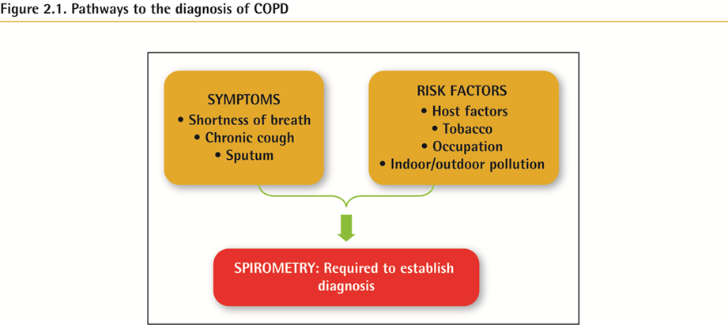
증상과 Risk Factor 가 있어 의심되는 상태에서 Spirometry 시행하여 Post-BDR FEV1/FVC 가 0.7 미만이면 COPD 로 진단이 가능하다. (최근에는 초기에 COPD 를 진단하여 치료를 빨리 시작하자는 움직임이 있고, Risk factor 가 알려지지 않은 요인도 있으므로, 증상과 Risk factor 가 없더라도 COPD 로 진단이 불가능한 것은 아니다.)
* 감별진단 : 천식, 울혈성심부전, 기관지 확장증, 결핵, 폐쇄성 기관지염 (Bronchiolitis obliterans) 미만성 세기관지염 등.
Classification of severity of airflow limitation
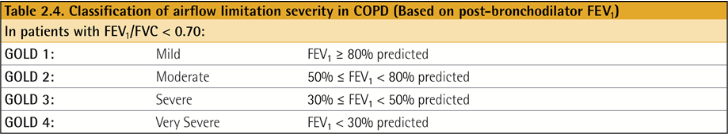
* FEV1 30/50/80% 기준으로 나뉘며 총 4가지 분류가 있다.
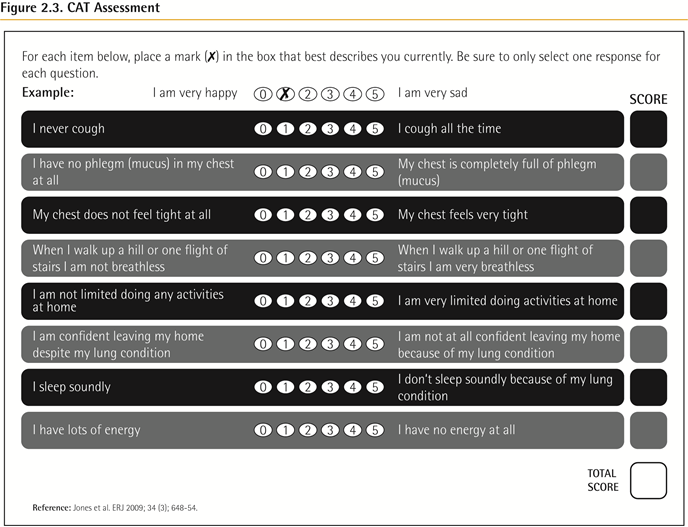
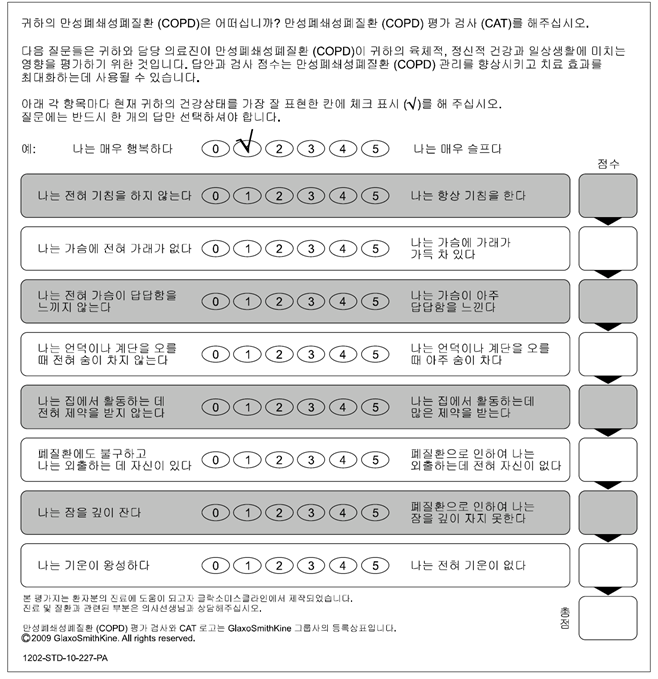
Choice of thresholds (증상 평가)
COPD Assessment Test (CAT)
Modified Medical Research Council (mMRC) questionnaire
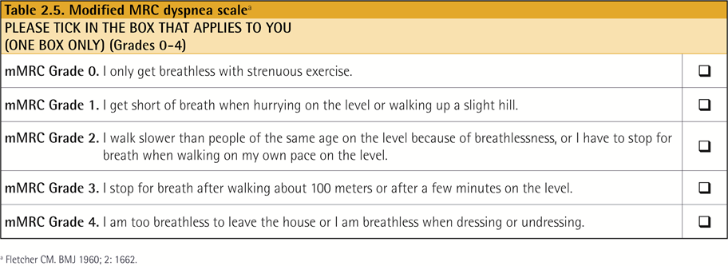
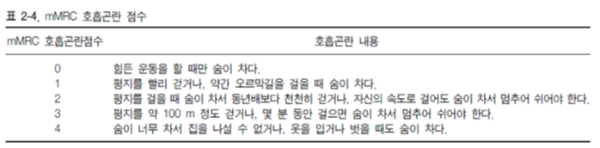
* mMRC 2 부터 증상이 심하다고 보기 때문에 2점을 잘 알고 있어야 한다.
Assessment of Exacerbation Risk (악화위험도 평가)
An exacerbation of COPD is defined as an acute worsening of respiratory symptoms that results in additional therapy. COPD exacerbations are defined as an acute worsening of respiratory symptoms that result in additional therapy.
빈번한 악화 (연간 2회 이상) 의 가장 좋은 예측 인자는 과거 악화 병력.
ABCD Assessment Tool
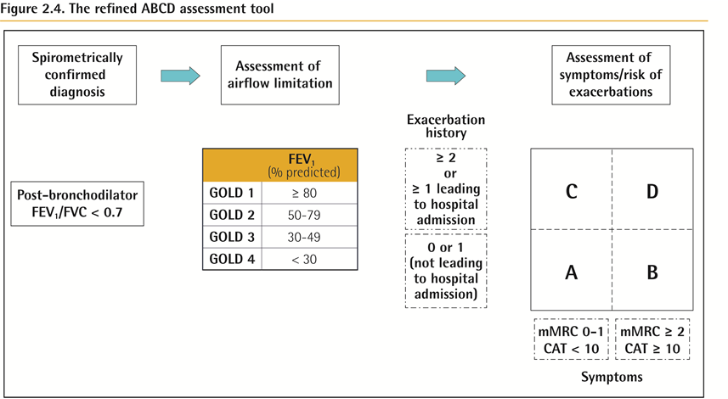
Example :
Consider two patients:
Both patients with FEV1 < 30% of predicted
Both with CAT scores of 18
But, one with 0 exacerbations in the past year and the other with 3 exacerbations in the past year.
Both would have been labelled GOLD D in the prior classification scheme.
With the new proposed scheme, the subject with 3 exacerbations in the past year would be labelled GOLD grade 4, group D.
The other patient, who has had no exacerbations, would be classified as GOLD grade 4, group B.
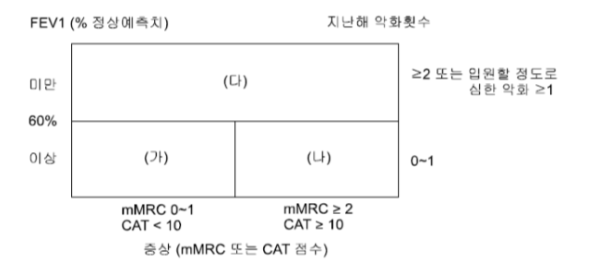
* 우리나라의 경우 FEV1 60% 기준으로 (가)(나) / (다) 를 나누었다.
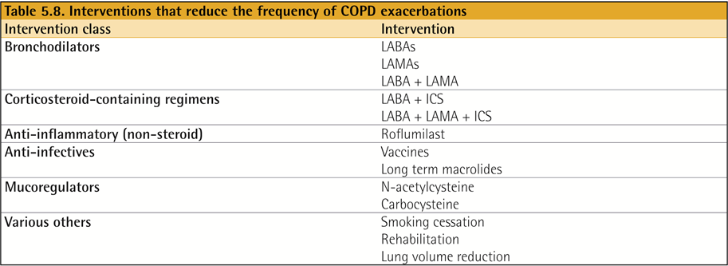
Evidence Supporting Prevention & Maintenance Therapy
흡연 중단은 만성 폐쇄성 폐질환(COPD) 관리에서 핵심 요소입니다. 약물 치료와 니코틴 대체 요법은 장기적인 금연 성공률을 안정적으로 증가시킵니다. 전자담배의 금연 보조 수단으로서의 효과와 안전성은 현재로서는 불확실합니다.
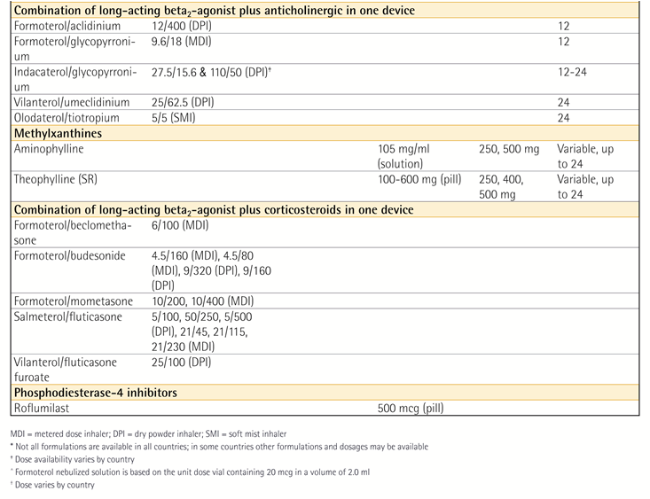
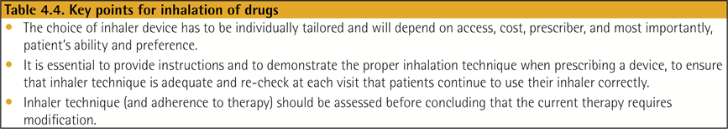
약물 치료는 COPD 증상을 완화하고, 악화 빈도 및 중증도를 줄이며, 건강 상태와 운동 내성을 향상시킬 수 있습니다. 약물 치료는 증상의 중증도, 악화 위험, 부작용, 동반 질환, 약물의 가용성과 비용, 환자의 반응 및 선호도, 흡입기 사용 능력 등을 고려하여 개별화되어야 합니다. 흡입기 사용법은 정기적으로 평가되어야 합니다.
인플루엔자 백신은 하기도 감염의 발생률을 감소시킵니다. 폐렴구균 백신은 하기도 감염의 빈도를 감소시키며, PCV13과 PPSV23 백신은 65세 이상 모든 환자에게 권장됩니다.
폐 재활 치료는 증상, 삶의 질, 그리고 일상 활동에서의 신체적·정서적 참여를 향상시킵니다.
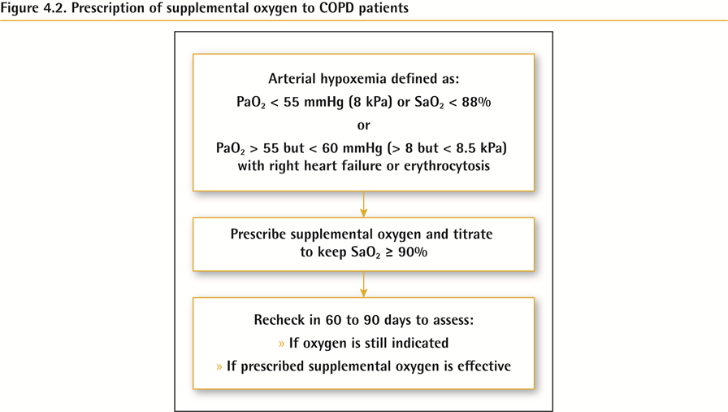
중증의 안정적인 만성 저산소혈증이 있는 환자에서는 장기 산소 요법이 생존율을 향상시킵니다.
안정적인 COPD 환자 중 안정 시 또는 운동 시 중등도의 산소포화도 저하가 있는 경우에는 산소 치료를 일률적으로 시행하지 않아야 합니다. 그러나 개별 환자의 상태에 따라 보조 산소의 필요성을 평가해야 합니다.
중증 만성 고탄산혈증이 있고 급성 호흡 부전으로 입원 병력이 있는 환자의 경우, 장기적인 비침습적 환기 요법은 사망률을 낮추고 재입원을 예방할 수 있습니다.
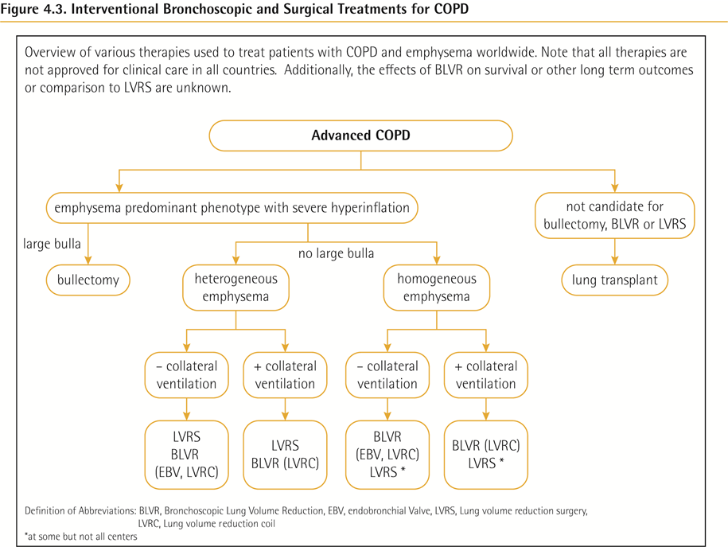
최적화된 내과적 치료에 반응하지 않는 진행된 폐기종 환자 중 일부에서는 외과적 또는 기관지 내 중재적 치료가 도움이 될 수 있습니다.
말기 COPD 환자에게는 완화 치료가 증상 조절에 효과적입니다.
Pharmacologic Therapy
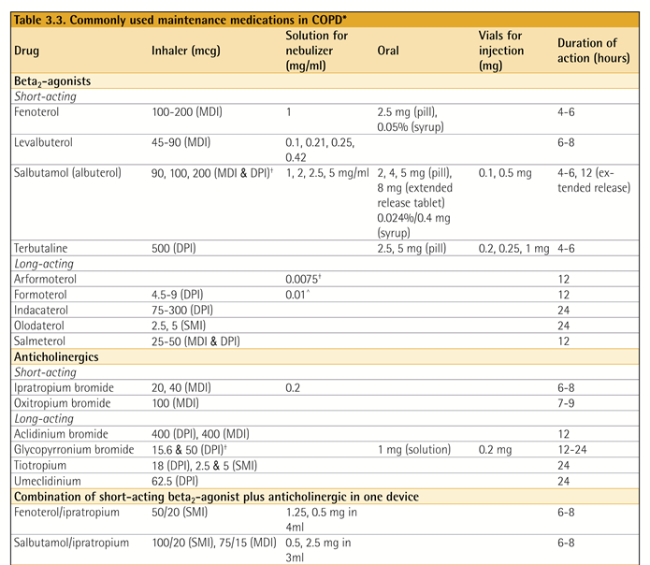
* Inhaler 종류
- Onbrez breezhaler – indacaterol maleate (LABA)
- Ventolin nebules – salbutamol (SABA)
- Ventolin evohaler – salbutamol (SABA)
- Alvesco – ciclesonide (ICS)
- Budecort – budesonide (ICS)
- Atrovent – ipratropium (SAMA)
- Spiriva respimat – tiotropium (LAMA)
- Spiriva handihilar – tiotropium (LAMA)
- Anoro – vilanterol, umeclidinium (LABA + LAMA)
- Flutiform inhaler – fluticasone, formoterol (ICS + LABA)
- Foster – beclomethasone, formoterol (ICS + LABA)
- Seretide – Salmeterol, fluticasone (ICS + LABA)
- Symbicort – budesonide, fomoterol (ICS + LABA)
- Xoterna breezhaler – indacaterol, glycopyrronium (LABA + LAMA)
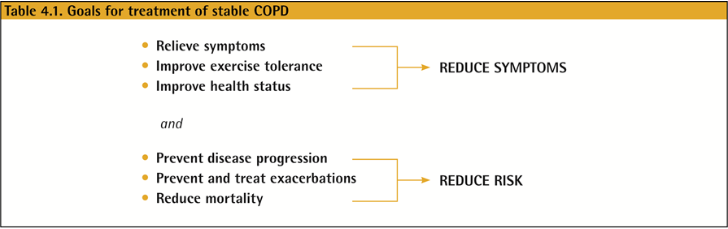
Management of Stable COPD
Once COPD has been diagnosed, effective management should be based on an individualized assessment to reduce both current symptoms and future risks of exacerbations.
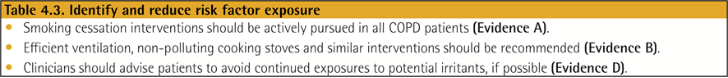
Identify and reduce exposure to known risk factors (s)
Identification and reduction of exposure to risk factors is important in the treatment and prevention of COPD.
Cigarette smoking is the most commonly encountered and easily identifiable risk factor for COPD, and smoking cessation should be continually encouraged for all individuals who smoke.
Reduction of total personal exposure to occupational dusts, fumes, and gases, and to indoor and outdoor air pollutants, should also be addressed.
Pharmacologic treatment (s)
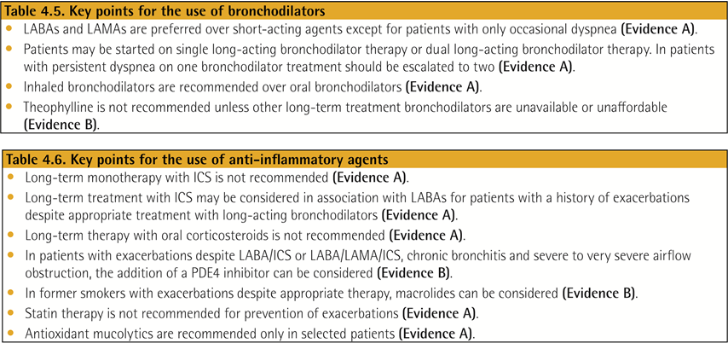
Pharmacologic therapies can reduce symptoms, and the risk and severity of exacerbations, as well as improve health status and exercise tolerance.
Most of the drugs are inhaled so proper inhaler technique is of high relevance.
Pharmacologic treatment algorithms
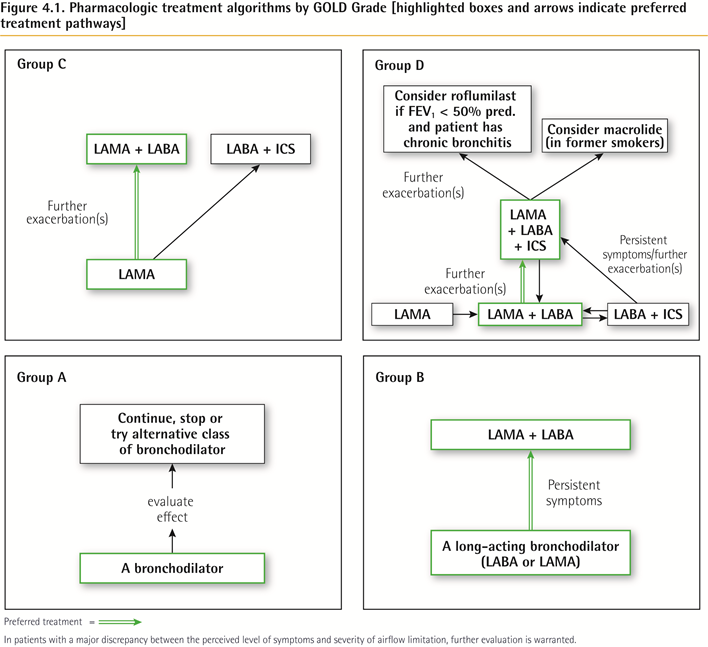
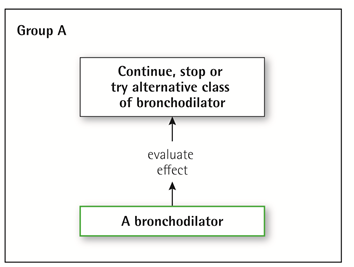
Group A
All Group A patients should be offered bronchodilator treatment based on its effect on breathlessness. This can be either a short- or a long-acting bronchodilator.
This should be continued if symptomatic benefit is documented.
Group B
Initial therapy should consist of a long acting bronchodilator. Long-acting inhaled bronchodilators are superior to short-acting bronchodilators taken as needed i.e., pro re nata (prn) and are therefore recommended.
There is no evidence to recommend one class of long-acting bronchodilators over another for initial relief of symptoms in this group of patients. In the individual patient, the choice should depend on the patient’s perception of symptom relief.
For patients with persistent breathlessness on monotherapy the use of two bronchodilators is recommended.
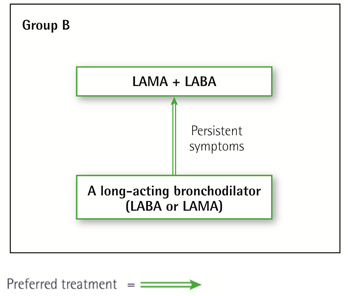
For patients with severe breathlessness initial therapy with two bronchodilators may be considered.
If the addition of a second bronchodilator does not improve symptoms, we suggest the treatment could be stepped down again to a single bronchodilator.
Group B patients are likely to have comorbidities that may add to their symptomatology and impact their prognosis, and these possibilities should be investigated.
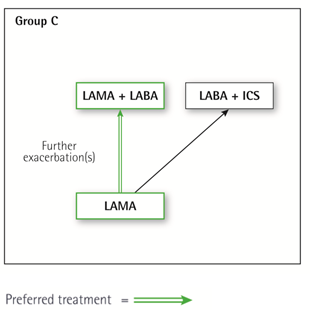
Group C
Initial therapy should consist of a single long acting bronchodilator. In two head-to head comparisons the tested LAMA was superior to the LABA regarding exacerbation prevention, therefore we recommend starting therapy with a LAMA in this group.
Patients with persistent exacerbations may benefit from adding a second long acting bronchodilator (LABA/LAMA) or using a combination of a long acting beta2-agonist and an inhaled corticosteroid (LABA/ICS). As ICS increases the risk for developing pneumonia in some patients, our primary choice is LABA/LAMA.
Group D
We recommend starting therapy with a LABA/LAMA combination because:
In studies with patient reported outcomes as the primary endpoint LABA/LAMA combinations showed superior results compared to the single substances. If a single bronchodilator is chosen as initial treatment, a LAMA is preferred for exacerbation prevention based on comparison to LABAs.
A LABA/LAMA combination was superior to a LABA/ICS combination in preventing exacerbations and other patient reported outcomes in Group D patients.
Group D patients are at higher risk of developing pneumonia when receiving treatment with ICS.
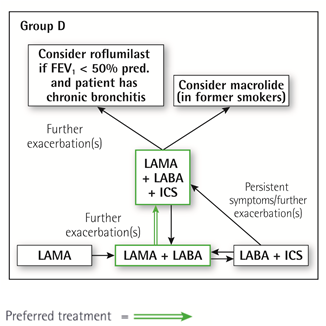
일부 환자에서는 초기 치료로 LABA/ICS 병합요법이 우선 선택이 될 수 있습니다. 이러한 환자들은 천식-COPD 중복(asthma-COPD overlap)을 시사하는 병력이나 검사 소견이 있을 수 있습니다. 또한, 혈중 호산구 수치가 높은 경우 흡입 코르티코스테로이드(ICS) 사용을 뒷받침하는 근거로 고려될 수 있으나, 이에 대한 논의는 아직 진행 중입니다.
LABA/LAMA 병합요법을 받는 중에도 악화가 지속되는 환자에서는 다음 두 가지 대안을 고려할 수 있습니다.
- LABA/LAMA/ICS로 단계 상승. 현재 LABA/LAMA와 LABA/LAMA/ICS의 악화 예방 효과를 비교하는 연구가 진행 중입니다.
- LABA/ICS로 전환. 그러나 LABA/LAMA에서 LABA/ICS로 전환하는 것이 더 나은 악화 예방 효과를 보인다는 근거는 없습니다. 만약 LABA/ICS 치료가 증상이나 악화에 긍정적인 영향을 주지 않는다면, LAMA를 추가할 수 있습니다.
LABA/LAMA/ICS 병합요법을 받는 환자에서도 악화가 지속된다면 다음 치료 옵션을 고려할 수 있습니다:
- 로플루밀라스트(roflumilast) 추가: FEV1이 예측치의 50% 미만이고 만성 기관지염이 있으며, 지난 1년 내에 악화로 입원한 병력이 있는 환자에게 특히 고려할 수 있습니다.
- 마크롤라이드(macrolide) 계열 항생제 추가: 가장 확실한 근거는 아지스로마이신(azithromycin)에 대해 보고되어 있습니다. 내성 균주의 발생 가능성도 치료 결정 시 함께 고려해야 합니다.
또한, ICS 중단도 고려할 수 있습니다. 효과 부족, 부작용 위험 증가(특히 폐렴), ICS 중단이 유해하지 않다는 증거에 기반하여 중단을 권고하는 경우도 있습니다.
Non-Pharmacologic Treatment
– 금연, 신체활동 권유, 예방주사 (독감, 폐렴알균) –> GOLD A/B/C/D
– 호흡재활 –> GOLD B/C/D
Interventional bronchoscopy and surgery (s)
최적화된 내과적 치료에도 반응하지 않는 이질적 또는 동질적 폐기종과 의미 있는 과팽창이 있는 선별된 환자에서, 외과적 또는 기관지 내 폐용적 감소술(예: 기관지 일방향 밸브 또는 폐 코일)을 고려할 수 있습니다.
큰 공기낭이 있는 선별된 환자에서는 외과적 공기낭 절제술을 고려할 수 있습니다.
매우 중증의 COPD를 가지고 있으며 관련된 금기사항이 없는 선별된 환자에서는 폐이식을 고려할 수 있습니다.
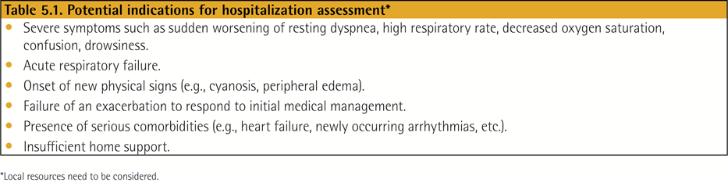
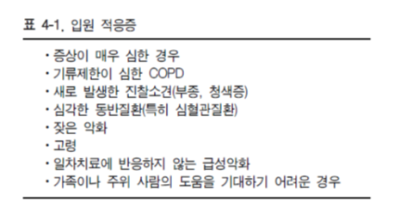
Management of Exacerbations
COPD의 급성 악화는 호흡기 증상의 급성 악화를 의미하며, 추가적인 치료가 필요한 상태로 정의됩니다.
COPD 악화는 여러 요인에 의해 유발될 수 있으며, 가장 흔한 원인은 호흡기 감염입니다.
급성 악화 치료의 초기 기관지 확장제로는 단기 작용 흡입성 베타2 작용제(벤토린)를 단독 또는 단기 작용 항콜린제(아트로벤트)와 병용하여 사용하는 것이 권장됩니다. (근거 수준 C)
장기 작용 기관지 확장제를 이용한 유지 치료는 가능한 한 조기에, 입원 퇴원 전 시작되어야 합니다.
전신 스테로이드는 폐기능(FEV1)과 산소화 개선, 회복 기간 및 입원 기간 단축에 효과가 있습니다. 치료 기간은 5~7일을 넘지 않아야 합니다. (근거 수준 A)
적절한 경우 항생제 사용은 회복 기간 단축, 조기 재발 및 치료 실패 위험 감소, 입원 기간 단축에 효과가 있습니다. 치료 기간은 5~7일이 적절합니다. (근거 수준 B)
메틸잔틴계 약물은 부작용 위험이 높기 때문에 권장되지 않습니다. (근거 수준 B)
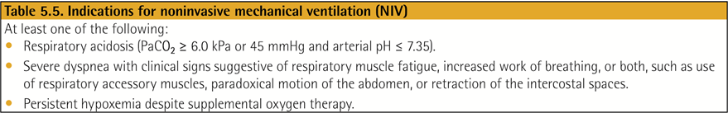
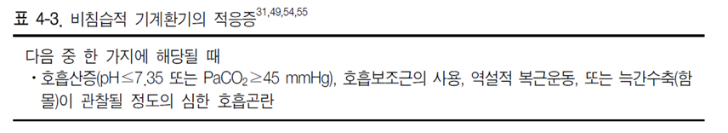
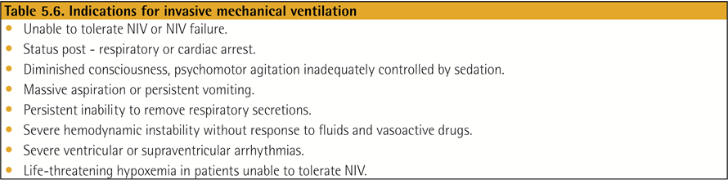
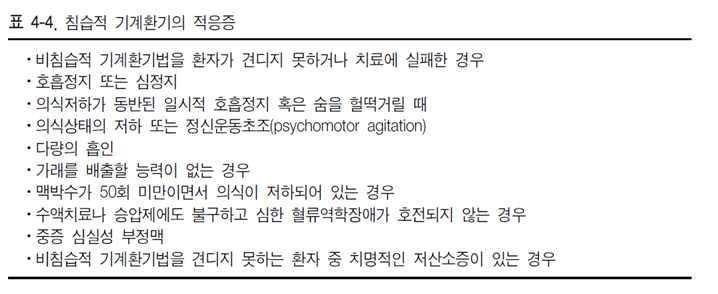
비침습적 기계 환기는 절대적 금기 사항이 없는 COPD 환자의 급성 호흡부전 치료에서 1차 선택이 되어야 합니다. 이는 가스 교환 개선, 호흡 노력 감소, 삽관 필요성 감소, 입원 기간 단축 및 생존율 향상에 효과가 있습니다. (근거 수준 A)
Pharmacologic treatment (s)
The three classes of medications most commonly used for COPD exacerbations are:
Bronchodilators
Although there is no high-quality evidence from RCTs, it is recommended that short-acting inhaled beta2-agonists, with or without short-acting anticholinergics, are the initial bronchodilators for acute treatment of a COPD exacerbation.
Corticosteroids
Data from studies indicate that systemic glucocorticoids in COPD exacerbations shorten recovery time and improve lung function (FEV1). They also improve oxygenation, the risk of early relapse, treatment failure, and the length of hospitalization.
Antibiotics
** COPD 급성 악화에서 IV aminophylline 의 role 은 줄어들고 있다.
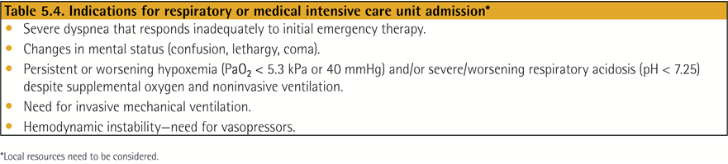
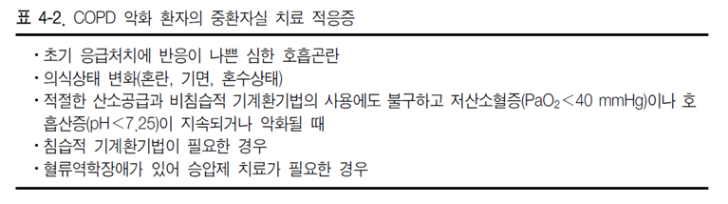
Respiratory support